Cardiogenic Shock Math
Goal values
Cardiac index (CI): > 2.2 lpm/m2,
Systemic vascular resistance (SVR): 800-1200 dynes/s/cm2,
Central venous pressure (CVP): 8-12 mmHg.
Fick CI/CO Derivation
Where, [math]C_a and C_v[/math] are derrived from the Oxygen content equation:
[math]CO_2 = \frac{1.34mLO_2}{gHb} * Hb * SaO_2 + 0.0031*PaO_2[/math],
Hb is in g/dL; to convert to g/L:
[math]CO_2 = \frac{1.34mLO_2}{gHb} * Hb * 10* SaO_2 + 0.0031*PaO_2[/math],
[math]\Longrightarrow[/math]
[math]CO_2 = \frac{13.4mLO_2}{gHb} * Hb * SaO_2 + 0.0031*PaO_2[/math],
The [math]0.0031*PaO_2 [/math] is negligible and can be removed,
[math]\therefore[/math]
[math]CI = \frac{VO_2}{13.4 \times Hb \times (\frac{SaO_2 – SvO_2}{100})}[/math],
[math]CO = CI \times BSA [/math]
BSA = Body surface area, CI = Cardiac index, CO = Cardiac output, CO2 = oxygen content, Ca = oxygen content in artery, Cv = oxygen content in venous system, Hb = hemoglobin, SaO2 = Oxygen saturation in the artery, SvO2 = Oxygen saturation in the venous system, PaO2 = Partial pressure of oxygen in blood, VO2 = Oxygen consumption.
Cardiac Index Calculator
Notes
- SvO2 is usually the PA Sat obtained from a pulmonary artery catheter. You can also use the SVC or right atrial sat obtained from a central line.
- You can use the Art Sat from a pulse oximeter, but the most accurate would be the saturation of arterial blood gas.
- Indexed VO2 of 125 ml/min/m2 is an estimated value from Dehmer and colleagues. For the elderly, you can also use 110 ml/min/m2, as demonstrated by Grafton and colleagues.
- Limitations of the Fick calculations are predominantly from the estimation of oxygen consumption from nomograms.
Systemic Vascular Resistance (SVR) Calculation
SVR Equation
[math]SVR(dynes/s/cm^{-5}) = 80\times \frac{MAP-CVP}{CO} [/math]
CO = Cardiac output, CVP = Central venous pressure, MAP = Mean arterial pressure, SVR = Systemic vascular resistance.
Notes
- Normal values are typically 800 – 1200 dynes/s/cm^-5
SVR Calculator
Pulmonary Artery Pulsatility Index (PAPi)
PAPi Calculation
[math] PAPi = \frac{PAs – PAd}{CVP} [/math], <br><br>
PAs = Pulmonary artery systolic pressure, PAd = pulmonary artery diastolic pressure, CVP = Central venous pressure.
Notes
- PAPi is an indicator of RV function
- RVSP is an indirect indicator of RV contractile function given a specific afterload condition
- Higher RAP can suggest a failing RV
- PAPi is dependent on loading conditions, i.e., PA capacitance, PA pulse pressure, stroke volume, and RAP
- PA capacitance = stroke volume / PA pulse pressure
- PA Capacitance is a measure of the RV’s ability to accommodate the blood ejected in systole
- Further reading: Lim et al.
PAPi Calculator
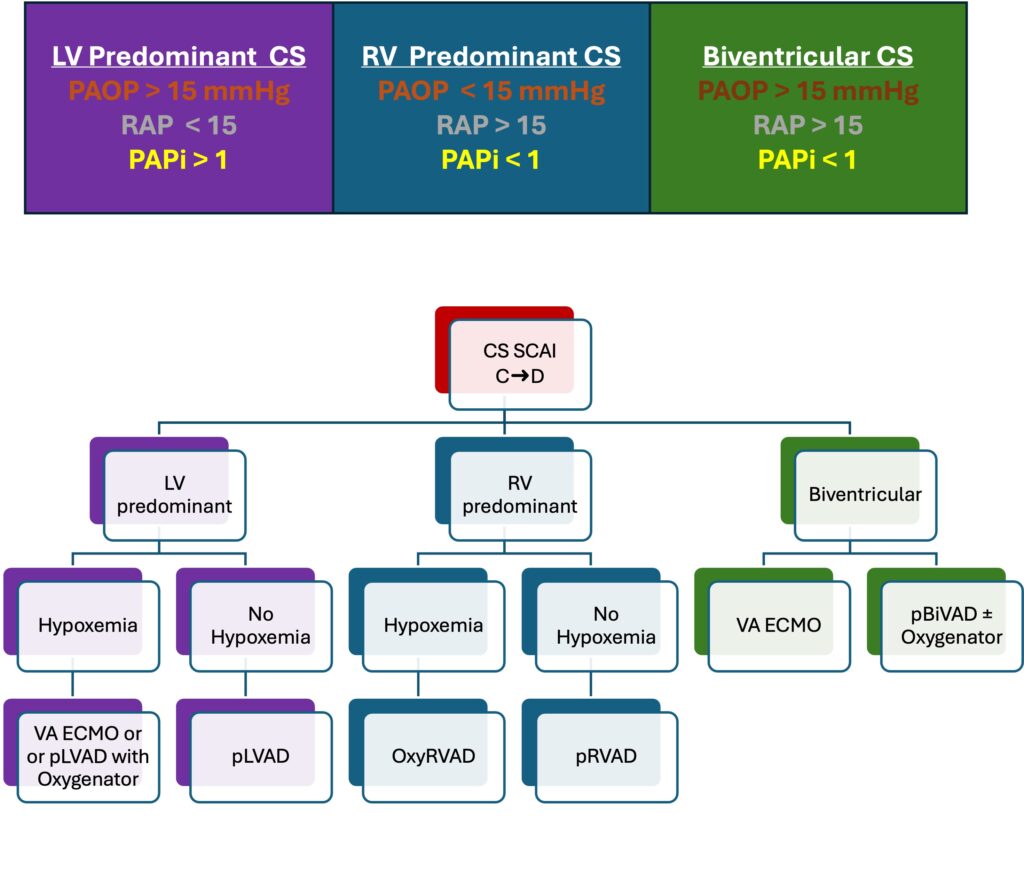
pLVAD = percutaneous LVAD such as an Abiomed Impella 5.5/CP
pRVAD = percutaneous RVAD such as a LivaNova ProTek Duo or an Abiomed Impella RP Flex.
- Oxygenators can be added to the ProTek but not the Impella RP Flex
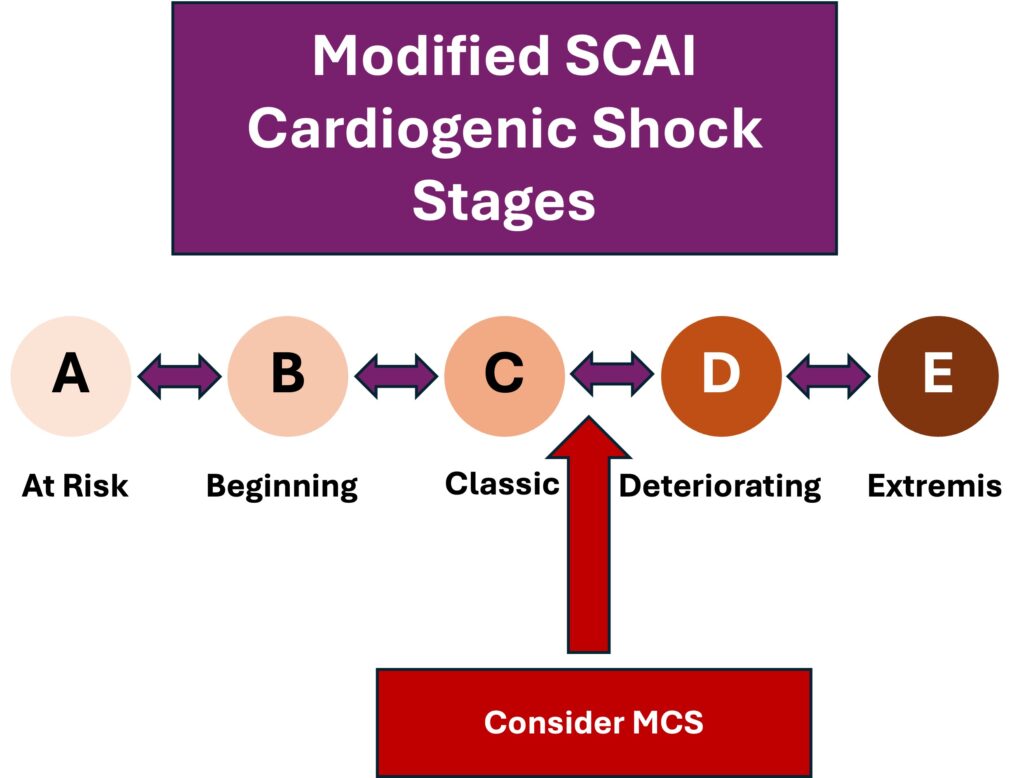
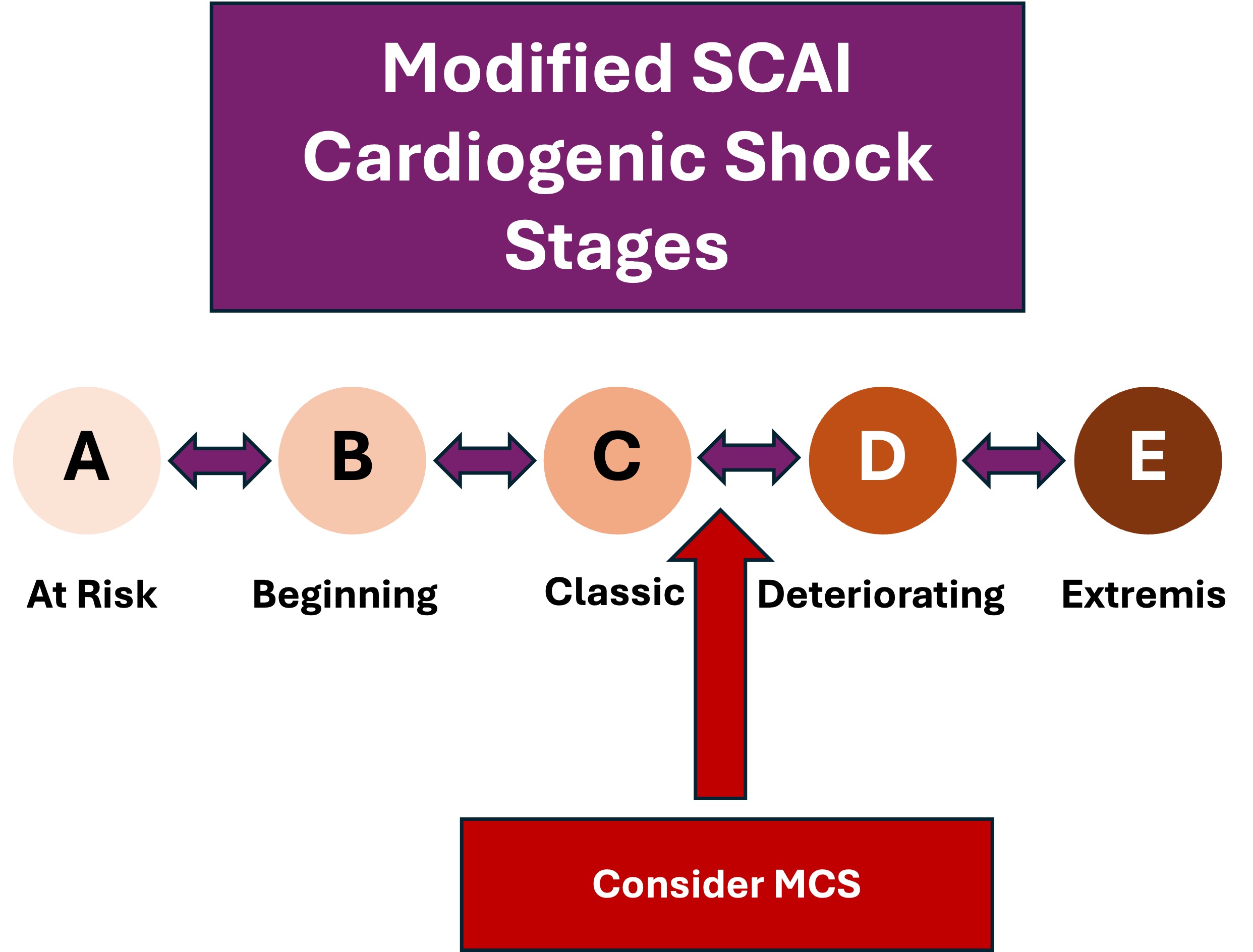
- Consideration for mechanical circulatory support (MCS) should be triggered when patients who present with classic shock are deteriorating with standard medical therapies (i.e., inotropes, vasodilators, and diuretics).
- A shock team approach should be considered. Papolos et al.
- Before initiation of MCS, contraindications and next-step strategies (i.e., bridge to permanent ventricular assist devices, transplant, palliation) should be considered.
Leave a Reply
You must be logged in to post a comment.